COVID-19’s Impacts on The Brain and Mind Are Varied and Common – New Research
The coronavirus' neurological and psychiatric impacts are likely to pose a challenge to clinicians and healthcare systems for many years to come.
Although COVID-19 was first described as a disease of the lungs, as its relentless march has continued we’ve realised that it has a far wider reach in the human body. COVID-19 has been associated with skin rashes, bleeding disorders and structural damage to the heart and kidneys. It has also been implicated in disorders of both the brain and the mind.
Early studies prompted fears that healthcare services would collapse under a crushing wave of strokes, brain inflammation and muscular disorders. Moreover, reviews of previous coronavirus outbreaks warned that those recovering from COVID-19 may face an increased burden of psychiatric disorders like depression and PTSD.
But despite research on COVID-19 and the brain being produced at unprecedented scale and speed during the pandemic – with hundreds of new articles appearing every week – it was hard initially to find reliable data to confirm or disprove these fears.
So, as a team of doctors, students and researchers from disciplines including psychiatry, psychology and neurology, we joined forces to analyse all the available research on the effects of COVID-19 on the brain. By doing so, we aimed to cut through a lot of the speculation surrounding COVID-19’s neurological and psychiatric effects. Here’s what we found.
Different conditions, different frequencies
Our team soon realised that many of the associations between COVID-19 and the brain were being drawn from small, highly selected groups of patients, which risks bias. So to combat this, we whittled down the vast number of potentially relevant papers on the neurology and psychiatry of COVID-19 (more than 13,000) to 215 that were robust enough to be analysed. Collectively, these covered 105,000 people from 30 countries.
We found that in these studies the most common neuropsychiatric symptoms were loss of smell (anosmia), weakness, fatigue and a change in taste (dysgeusia), which all happen quite frequently. Anosmia and weakness appeared in more than 30% of the patients the studies we looked at, for example. It’s therefore very likely that neuropsychiatric symptoms in COVID-19 are the rule and not the exception.
But reassuringly, initial fears about more serious brain-related conditions – such as widespread inflammation of the brain (encephalitis) and Guillain-Barré syndrome, where the immune system attacks the nerves – seemed to be based only on very rare events. Concerns about vast waves of such conditions seem unfounded.
However, we did find that some important mental illnesses, such as depression and anxiety, were each occurring in as many as 25% of people with COVID-19. These may represent a huge burden to patients in years to come. Even neurological events reported less frequently, like stroke (which occurred in about 2% of hospitalised patients), will still represent an enormous challenge to patients and healthcare systems due to the sheer scale of this pandemic’s reach and the fact that they often have life-changing results.
Interestingly, we found that several symptoms (including muscle pain and loss of smell) were actually reported more commonly in those with less severe COVID-19 – the opposite of what you might expect. Of course, there may be a simple explanation for this: perhaps critically unwell patients are less likely to be probed about certain symptoms, particularly those that are less severe. We also saw many disabling symptoms (including fatigue and headache) present in those who were not hospitalised at all.
But answers are far from final
While reading this, you may have been struck by a big question surrounding all these studies: how do we know that COVID-19 is actually causing any of these problems? Depression is common – might these people have developed it anyway without getting COVID-19? And what if having a psychiatric illness makes you more likely to get COVID-19? One large study with US data suggests that this is the case.
These are all real issues in the data available up to this point, as unless you have a comparison group of individuals without COVID-19, it’s impossible to know whether the people you are studying were going to have high rates of neuropsychiatric disorders regardless of catching the coronavirus. Ideally, you need a group of people without mental illness as your baseline, and to then see what happens when some of them are exposed to COVID-19.
Without such studies, it’s hard to draw any hard conclusions – and unfortunately almost all of the studies we looked at didn’t have comparison groups. However, we’re starting to get some comparative data now. For example, we now know that people who have had COVID-19 are more likely than the general population to develop a new mental illness. In addition, most psychiatric and neurological problems seem to be more common after COVID-19 than after flu.
Another issue is that the research done so far contains biases that can’t be eliminated. It’s biased towards patients in hospital, when most people with COVID-19 never go near a hospital. It’s biased towards acute illness, rather than the longer-term effects of COVID-19. And it’s biased towards China, the US and other western countries, with little known about what is happening in Africa or much of the Pacific region. To get a more comprehensive view, we need future research to have a wider scope.
What we do know is that people with COVID-19 very often experience a range of neurological and psychiatric problems, so healthcare providers need to prepare not only for the immediate care of these patients, but also the intensive and often lengthy rehabilitation needs that follow. Early research (yet to be reviewed by other scientists) is raising concerning signs of neuropsychiatric symptoms persisting many months following the onset of illness.
Finding out the true impact of COVID-19 on the brain is only a first step. In reality, the disease’s neurological and psychiatric impacts are likely to pose a challenge to clinicians and healthcare systems for many years to come.
Cameron Watson is a Junior Doctor and Dementia Researcher, Wolfson Institute of Preventive Medicine, Queen Mary University of London
Jonathan Roger is a Wellcome Trust Clinical Fellow in Psychiatry, UCL
This article is republished from The Conversation under a Creative Commons license. Read the original article.
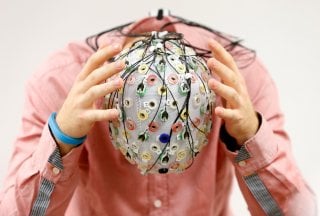
Image: Reuters